While visiting temple, Ms Bui Thi Tho (94 years old, residing in Da Lat) suddenly felt dizzy and collapsed. She was taken to a local hospital discharged and two days later, but fainted again soon after. Her family brought her to FV Hospital’s Accident and Emergency (A&E) Department for urgent care.

Ms Tho and Dr Hoang Quang Minh, FV Hospital
Overcoming the difficulty of finding the correct direction to save a patient when their pacemaker has malfunctioned
Dr Hoang Quang Minh, Cardiology Senior Consultant, FV Hospital, found that at the beginning of January 2023, patient Bui Thi Tho was given emergency care in a dangerous condition. Her risk of sudden death was very high as Ms Tho was elderly, had many underlying diseases and was completely dependent on a pacemaker. Ms Tho suffered from a long-standing third-degree atrioventricular block. Although she has had a pacemaker inserted twice, a left ventricular single-chamber machine, there was still no synchronisation between the atrial and ventricular wires. This situation could easily lead to heart failure.
When examining Ms Tho’s pacemaker history, the doctor discovered tachycardias had occurred at the time she fainted. “The question is: Why does the patient who has a pacemaker still have these symptoms? We performed a coronary artery examination, but the patient did not have coronary artery stenosis,” says Dr Minh.
“The patient said that when she did specific activities, she often fainted or became dizzy. Therefore, we asked Ms Tho to perform some of these activities in a safe, controlled environment at FVH and found that her pacemaker was not working. This proved that the pacing wire is faulty, and that it was necessary to replace the pacing wire or implant another pacing system entirely to ensure Ms Tho’s safety.”
This was a particularly difficult case as Ms Tho was 94 years of age and has many underlying diseases, including blood pressure, diabetes, and level 2 kidney failure. A surgical plan to address her faulty pacemaker required doctors to minimise the number of invasive surgeries to ensure Ms Tho’s safety.
Doctors proposed two options: One, to replace the wire and keep the machine in its old position; second, to move the old pacemaker to a new location, and then insert a new pacemaker wire through a new vein.
“However, when the patient already has a wire in the subclavian vein, the diameter of the vein will be very small. Putting a new pacemaker wire on top of an old one is very difficult, and the risk of complications is high. Even if the surgery is successful, the patient’s activities would still be limited with zero improvement,” adds Dr Minh.
“If it is not possible to replace the wire in the old position, it is necessary to perform a minor surgery to remove the old pacemaker and attach the new wire to it, which means we would have to make two incisions, one on each side.”
A wireless artificial cardiac pacemaker with atrial sensor – the optimal solution for a 94-year-old patient
After careful consideration, FV Hospital’s Cardiology doctors decided on a third option: to install a new-generation wireless artificial cardiac pacemaker with an atrial sensor. This is a small capsule-like device (one-tenth the size of a wired pacemaker) that is inserted directly into the patient’s heart chamber without the need for wiring.
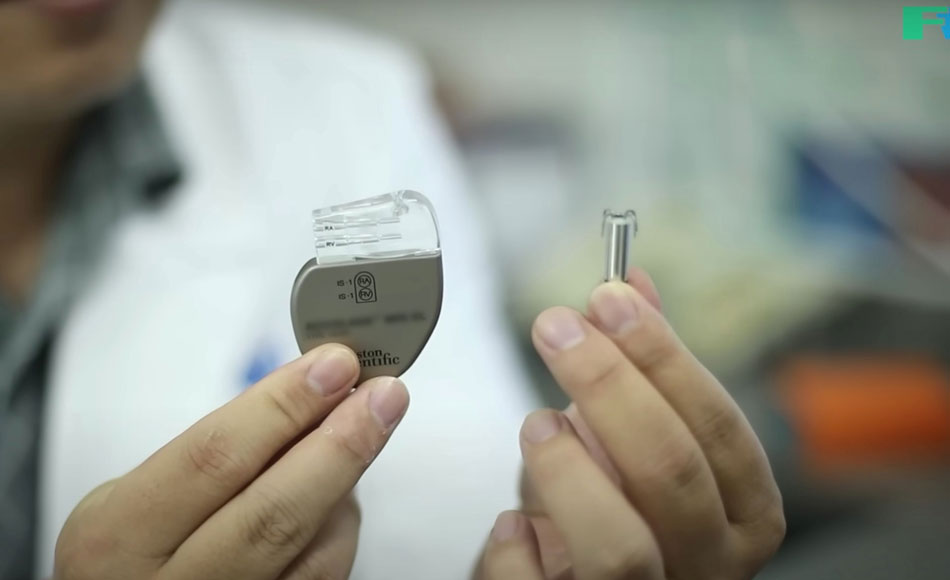
The wireless artificial cardiac pacemaker with atrial sensor, shown right, is a small capsule
The wireless artificial cardiac pacemaker with atrial sensor can achieve the same function as the wired machine with the optimal function of sensing and correcting trial chamber activity, thereby helping the atrial and ventricular chambers synchronise.
Dr Minh explains: “This solution means that the patient does not need a surgery to remove the old pacemaker. We will reduce the frequency of the wired machine and leave it in the sensing system, not pacing, and then insert the atrial chamber-sensing wireless pacemaker directly into the heart chambers.
“This also makes it possible for the patient to have an MRI scan without the interference of a new wire replacement option. However, as this is a new technique being applied in Vietnam, only doctors with a high level of technical expertise and access to the latest technology can perform it.”

Dr Minh examines Mr Tho after her surgery
To perform this delicate operation, the patient is anaesthetized before the doctor skillfully inserts the wireless artificial cardiac pacemaker directly into the heart chamber via a catheter through the femoral vein, dropping it into position near the current pacemaker wire. This is a minimally invasive procedure that requires less time to recover from that traditional pacemaker implantation.
Ms Tho’s surgery ended in success after 30 minutes and she recovered quickly; the next day she was able to stand up, go to the toilet and even do gentle exercise unaided.
After two days at FV Hospital, Ms Tho was discharged. She was monitored weekly for the first month after her surgery. All indicators and results were extremely positive, and she is in good health. This treatment has improved Ms Tho’s quality of life dramatically. Previously, she became fatigued from walking for one minute; now, she is more active and can do light exercises without worrying about losing consciousness.

Ms Tho was discharged from the hospital with a bright smile, much to the joy of her family
Ms Tho was excited to share how she felt on the day she was discharged from the hospital. “I feel fine, the wound is not painful, the doctors and nurses here have taken good care of me. In the new year, I hope to enjoy good health so that I can travel more and visit more temples”.
According to Dr Minh, implanting a wired pacemaker in a patient’s chest area can incur the risk of any movement causing bleeding, displacement and repair procedures, or even infection; it can also take a patient four weeks to recover from the surgery before they can return to their daily routine. However, after receiving a wireless artificial cardiac pacemaker with atrial sensor, Ms Tho was able to perform her daily personal activities immediately – a huge benefit of this device. In addition, compared with a wired pacemaker, the wireless artificial cardiac pacemaker helps to reduce the high risk of infection and post-operative scar discomfort; and is safer and causes less scarring.
However, for successful installation of a wireless artificial cardiac pacemaker, the surgeon must by highly experienced and fully certified to program and insert the device, and be able to take care of patients after surgery. Only when a doctor ticks all of these boxes will a supplier allow the doctor to implant its device. FV Hospital fully meets all of the above requirements.
Dr Minh says: “In May 2022, FV successfully placed a wireless artificial cardiac pacemaker with atrial sensor in an 88-year-old-patient – the oldest person in Vietnam to receive the surgery at that time. Now, at the age of 94, Ms Tho is our second successful case treating a patient of advanced years. Due to its outstanding advantages, a wireless artificial cardiac pacemaker is considered an optimal solution for controlling arrhythmias in cardiovascular patients with risk factors.”
To reduce costs for patients, FV Hospital cooperates with Ho Chi Minh City Social Insurance to expand the scope of the application of medical examination and treatment by State Health Insurance (HI) for high-tech treatment services at FV’s Interventional Catheterisation (Cathlab).
Services and procedures on the technical list approved by the social insurance agency include:
- Imaging and intervention to remove cerebral artery thrombosis, digitally erasing the background
- Background digitised angiography (DSA)
- Electrophysiological exploration and treatment of arrhythmias with conventional high-frequency waves
Patients can be covered by social insurance up to 45 per cent of the treatment cost at FV hospital. For more information, please contact: (028) 54 11 33 33.



