“It’s amazing! If I had known earlier, I wouldn’t have had to endure chest pain and shortness of breath for the past 17 years,” shared patient Nguyen Quang Thanh after receiving treatment.
Previously, the progression of hypertrophic cardiomyopathy had caused Mr Nguyen Quang Thanh (68 years old, from Binh Dinh) to suffer from severe mitral valve regurgitation, arrhythmia, chest pain, and shortness of breath for 17 years. After just one hour of undergoing alcohol septal ablation at FV Hospital, Mr Thanh could breathe easily, and his mitral valve regurgitation disappeared.

Patient Nguyen Quang Thanh poses for a photo with Ho Minh Tuan, MD, PhD before discharge
17 years of chest pain and shortness of breath due to hypertrophic cardiomyopathy
In 2007, Mr Nguyen Quang Thanh began experiencing prolonged fatigue and shortness of breath. He went for a check-up and was diagnosed with hypertrophic cardiomyopathy. Due to the provincial hospital’s lack of resources to treat this condition, the doctors advised him to seek treatment at higher-level hospitals.
He visited a hospital in Ho Chi Minh City and was prescribed medication. However, his shortness of breath and chest pain continued to worsen, leaving him constantly exhausted. He sought help from various hospitals and cardiology clinics, but none could offer him a viable treatment.
By chance, he came across an article written by Ho Minh Tuan, MD, PhD and his colleagues about the treatment methods for hypertrophic cardiomyopathy. “The symptoms described in the article were exactly what I was experiencing, not missing a single detail, so I was determined to find Dr Tuan,” Mr Thanh recalled.
In June 2024, Mr Thanh visited FV Hospital, where he was examined by Ho Minh Tuan, MD, PhD, Head of Cardiology Department. Dr Tuan measured that the thickness of Mr Thanh’s heart muscle had reached 23 mm, obstructing the left ventricular outflow and causing grade 4 mitral valve regurgitation. Without thorough treatment, the chest pain and shortness of breath would worsen, potentially leading to sudden death.
Dr Tuan explained that there were two treatment options for Mr Thanh: open-heart surgery to remove the thickened heart muscle or an intervention to reduce the thickness of the heart wall using alcohol septal ablation. Open-heart surgery is a major, complex operation and not all patients are suitable candidates. Therefore, Dr Tuan recommended the alcohol septal ablation method for Mr Thanh.
“Reducing the thickness of the heart wall with bioethanol is a percutaneous catheter-based intervention. The patient receives a catheter into a small peripheral blood vessel in the wrist or thigh. The doctor then threads a wire with an attached balloon containing absolute ethanol to the blood vessel supplying the thickened heart muscle. Once the correct blood vessel is located, ethanol is injected to blockage in the vessel, causing the thickened heart muscle to thin out,” Dr Tuan explained.

Dr Ho Minh Tuan and his team performed the alcohol septal ablation procedure to treat hypertrophic cardiomyopathy.
Mr Nguyen Quang Thanh underwent the alcohol septal ablation procedure performed by Dr Tuan’s team. The procedure took about one hour and required only local anaesthesia, allowing the patient to remain awake. The results were remarkable: the thickened heart muscle was significantly reduced, and the mitral valve regurgitation was resolved.

Ho Minh Tuan, MD, PhD examines the patient after the procedure.
“The intervention for Mr Nguyen Quang Thanh addressed two issues: the obstruction was reduced from 23 mm to just over 10 mm, and the mitral valve regurgitation decreased from grade 4 to grade 1. As a result, his symptoms of shortness of breath and chest pain were completely resolved,” said Dr Tuan.
Mr Thanh was discharged two days later, overjoyed that he could now breathe comfortably and easily. His treatment experience at FV was exceptional: Dr Tuan thoroughly explained my condition and the treatment method, which gave him great peace of mind. The procedure was quick and gentle. “The method is so complex, yet Dr Tuan performed it smoothly! During the procedure, I only felt chest discomfort for about 30 seconds, and there was no pain at all! It’s amazing! If I had known earlier, I wouldn’t have had to endure chest pain and shortness of breath for the past 17 years,” Mr Thanh said emotionally.
Treatment of hypertrophic cardiomyopathy: What should patients take note of?
Dr Tuan explained that hypertrophic cardiomyopathy is a common cardiac condition, often inherited or caused by genetic mutations, which results in abnormal thickening of the heart muscle. This condition can lead to obstruction of the left ventricular outflow tract, mitral valve regurgitation, diastolic dysfunction, myocardial ischemia, and arrhythmias.
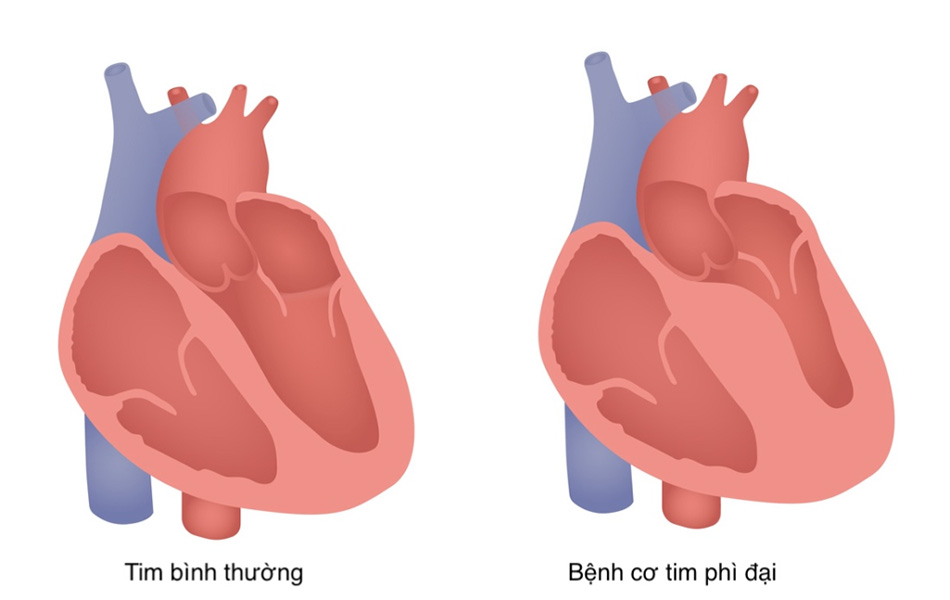
Illustration of a normal heart (left) and a heart affected by hypertrophic cardiomyopathy (right) with thickened heart walls.
Hypertrophic cardiomyopathy is categorised into two types: non-obstructive hypertrophic cardiomyopathy and obstructive hypertrophic cardiomyopathy. “Both types of hypertrophic cardiomyopathy can lead to arrhythmias and even sudden cardiac death. A notable example is athletes experiencing sudden death on the field, with up to 30% of young athletes’ deaths attributed to this condition,” explained Ho Minh Tuan. MD, PhD
To accurately diagnose hypertrophic cardiomyopathy, patients undergo examinations such as electrocardiography, echocardiography, and may have additional tests like CT or MRI scan of the heart. These imaging techniques help precisely detect the condition, specifically identifying heart wall thickness exceeding 15mm as diagnostic for hypertrophic cardiomyopathy.
This condition cannot be cured completely and may recur; the treatment goal is to help patients achieve a normal life and prolong lifespan. Patients with non-obstructive hypertrophic cardiomyopathy typically require medication. For those with obstructive hypertrophic cardiomyopathy, treatment involves a combination of medications and specialised techniques, such as the use of alcohol septal ablation as a prominent example.
The challenge of alcohol septal ablation lies in the high skill level required by the technicians. Initially, it involves pinpointing the exact branch of the blood vessel that supplies the thickened area of the heart causing obstruction. Once this tiny vessel is identified, the physician verifies its location by injecting contrast dye; if the thickened area of the heart lights up under imaging, it confirms correct identification. Subsequently, a special balloon with a diameter of 1-3 mm, containing absolute alcohol, is inserted into the blood vessel, blocking it and delivering the alcohol.
These procedures must be conducted meticulously to ensure the correct amount of alcohol is delivered. Otherwise, complications such as arrhythmias or alcohol leakage into other areas, leading to bleeding, may occur.
Moreover, this technique requires a state-of-the-art catheterisation laboratory (cathlab). Advanced equipment such as modern ultrasound machines, pressure measurement systems within the heart chambers and pacemaker devices provide the physician with precise parameters and clear images for accurate procedure execution.
“Alcohol septal ablation for hypertrophic cardiomyopathy has been practiced for many years and is widespread in many countries. However, there are still relatively few cardiovascular centres in Vietnam equipped to perform this procedure,” noted Dr Tuan.

FV Hospital is equipped with a modern Cathlab
The Cardiology Department at FV Hospital is equipped with a state-of-the-art Cath Lab, staffed by experienced doctors capable of providing comprehensive treatment for hypertrophic cardiomyopathy (HCM) across all age groups, from children to the elderly. Recently, FV Hospital has successfully performed dozens of procedures using alcohol septal ablation method.
After treatment, patients receive guidance on appropriate nutrition and exercise regimes. During follow-up visits, patients undergo cardiovascular fitness tests on a treadmill, allowing doctors to recommend suitable physical activity levels based on their health status. Regarding nutrition, patients are advised to follow a diet low in animal fats, quit smoking, limit alcohol consumption, and increase fish intake. Regular check-ups are essential.
Dr Tuan recommends that individuals with a family history of this condition undergo cardiac evaluations and regular check-ups every 3-5 years.



