Table of contents
- WHAT IS BENIGN PROSTATIC HYPERPLASIA (BPH)?
- WHAT IS PROSTATE ARTERY EMBOLISATION (PAE)?
- WHY MIGHT I NEED PROSTATE ARTERY EMBOLISATION?
- WHO HAS MADE THE DECISION?
- WHO WILL PERFORM THE PROCEDURE?
- HOW DO I PREPARE FOR PROSTATE ARTERY EMBOLISATION?
- WHAT HAPPENS DURING PROSTATE ARTERY EMBOLISATION?
- WILL IT HURT?
- HOW LONG WILL IT TAKE?
- WHAT HAPPENS AFTERWARDS?
- ARE THERE ANY RISKS?
- WHAT ARE THE RESULTS?
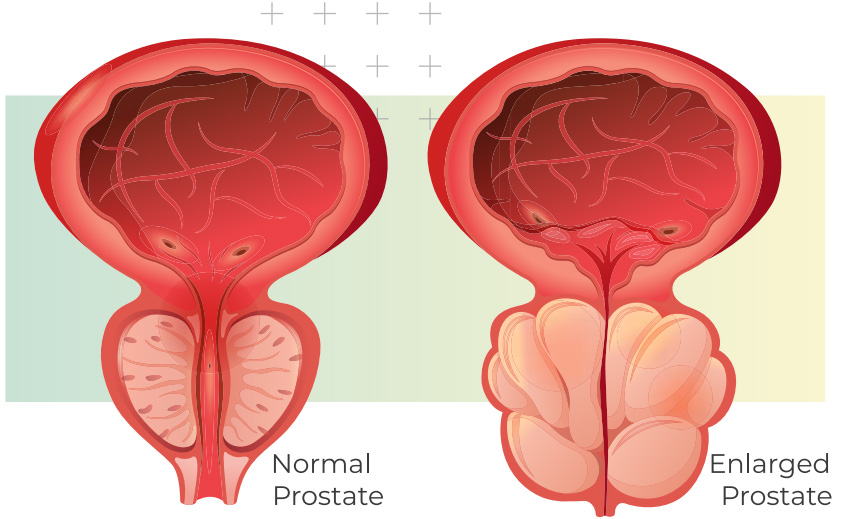
WHAT IS BENIGN PROSTATIC HYPERPLASIA (BPH)?
The prostate gland surrounds the outlet of a man’s bladder. BPH is a non-cancerous increase of prostate volume, and commonly causes obstruction of the bladder outflow. It is a very common condition in older men. By the age of 70, approximately 80% of men have an enlarged prostate.
In many men an enlarged prostate does not cause any problems. If symptoms do occur, they may include:
- Weak urine flow
- Sensation that the bladder is not empty after passing urine
- Increased frequency of urination with voiding small amounts of urine, particularly at night
- Urinary urgency with difficulty in controlling urination.
WHAT IS PROSTATE ARTERY EMBOLISATION (PAE)?
PAE is a non-surgical way of treating an enlarged prostate. The procedure works by blocking off the arteries that supply the gland, which makes it shrink. It is an alternative to having surgery to remove the prostate by the procedure called transurethral resection of prostate (TURP) or other prostate operations including laser surgery.
WHY MIGHT I NEED PROSTATE ARTERY EMBOLISATION?
Tests that you have done have shown that you have an enlarged prostate. Your symptoms may include passing urine very frequently (especially at night), passing only small volumes of urine and having a poor flow/stream of urine. PAE is a good option for those with a very big prostate gland, where treatment with medication or prostate operations (e.g. TURP or laser surgery) may not be successful or could have increased risks, and when symptoms are quite severe.
By shrinking the size of your prostate, PAE will help alleviate your symptoms.
WHO HAS MADE THE DECISION?
The urologist in charge of your case and the interventional radiologist who will perform the procedure will have discussed the situation and agreed that this may be the most suitable treatment for you. PAE has advantages versus TURP, including:
- Faster recovery time without hospitalisation
- Lower risk of complications
- Fewer or more minor complications.
However, the final decision is yours. We will only proceed with the procedure with your consent.
WHO WILL PERFORM THE PROCEDURE?
Specially trained doctors called interventional radiologists. Interventional radiologists are trained to perform various minimally-invasive procedures using medical imaging guidance, to diagnose, treat, and cure many kinds of conditions. They make small incisions and use needles and catheters to treat conditions inside your body.
The procedure takes place in a specialised X-ray room called a Cath-lab.
HOW DO I PREPARE FOR PROSTATE ARTERY EMBOLISATION?
The procedure is usually done as a day case, so you will not need to stay in hospital overnight.
You must stop eating 6 hours before the procedure, but you will still be able to drink clear fluids (water or squash) up to 2 hours before. You should take all of your normal morning medication on the day of the procedure, unless you have been given specific instructions not to do so.
When you arrive at the hospital, we will ask you to put on a hospital gown. As the procedure is generally carried out using the artery in the groin, we may ask you to shave the skin around this area.
Please let us know if you have any allergies or if you have previously reacted to intravenous contrast medium (the dye used for kidney X-rays and CT scanner).
WHAT HAPPENS DURING PROSTATE ARTERY EMBOLISATION?
PAE is done under local anaesthetic and, if required, intravenous sedative, allowing you to remain comfortable without the need for general anaesthesia.
You will lie on the Cath-lab machine table. A nurse will then insert a needle into a vein in your arm, so that the interventional radiologist can give you a sedative if required. Once the needle is in place, it should not cause you any pain.
A nurse will attach a monitoring device to your chest and finger and may also give you oxygen through a nose tube.
The interventional radiologist will keep everything sterile and will wear a theatre gown and operating gloves. The skin near the point of insertion, groin or wrist, will be swabbed with antiseptic and covered with a theatre drape.
The skin and deeper tissues over the artery in the groin or wrist will be anaesthetised with local anaesthetic, and then a needle will be inserted into this artery. Once the interventional radiologist is satisfied that this is correctly positioned, a guide wire is placed through the needle, and into this artery. Then the needle is withdrawn allowing a fine, plastic tube, called a catheter, to be placed over the wire and into this artery.
We will then use the X-ray equipment and a special dye (contrast medium) to make sure that the catheter and the wire are moved into the small arteries supplying the prostate. The dye may give you a warm feeling in your pelvis.
Once the catheter is in place, we will inject another fluid containing thousands of tiny particles through it into the prostate. This will block the small blood vessels within the prostate gland and starve it of its blood supply. The arteries on both the right and left side of the prostate will need to be blocked in this way. This can usually be done from the same incision in the groin. Occasionally it may be difficult to access both sides, so we may need to make a second incision at the top of your other leg.
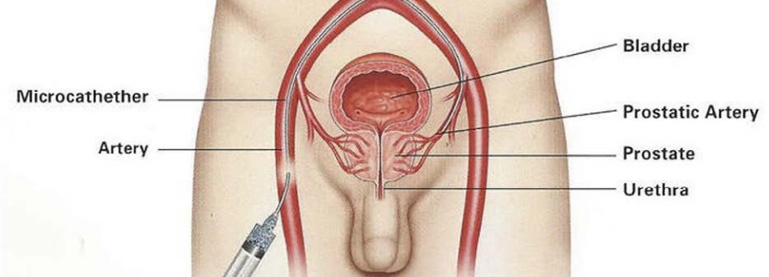
At the end of the procedure, we will remove the catheter, and the interventional radiologist will insert a closure device, and pressure will be applied to prevent any bleeding.
WILL IT HURT?
You may feel a slight sting when the local anaesthetic is injected, but this will soon pass. You may get a warm feeling as the special dye passes around your body, but this will also soon pass.
The procedure itself is not painful, but your doctor can sedate you if you become anxious.
HOW LONG WILL IT TAKE?
The procedure will be different for everyone, so it is not always easy to predict how long it will take. Most procedures are completed within 2 hours, but more complex cases can take 3 hours or longer. It is important that you empty your bladder before we begin. If you need to pass water (pee) during the procedure, please let us know.
WHAT HAPPENS AFTERWARDS?
After the procedure, we will take you to the recovery area, where nurses will carry out routine observations, such as taking your pulse and blood pressure. They will also check the skin entry point to make sure there is no bleeding.
We will then move you to the Day Ward, where you will stay in bed for a few hours to recover. We will usually send you home after four to 6 hours.
We will prescribe you antibiotics and painkillers if required and we will explain how to take them before you leave hospital.
Once you are home, you may feel tired and should rest for 2 to 3 days. You should be able to return to normal daily activities straight away. We recommend that you avoid any strenuous activity, including heavy lifting, for the first seven days.
ARE THERE ANY RISKS?
PAE has a very low complication rate.
There may occasionally be a small bruise, called a haematoma, at the site of needle puncture into the artery and this is quite normal. If this becomes a large bruise, then there is the risk of infection, and antibiotics maybe required.
You may experience some discomfort in the lower abdomen or when urinating, this normally resolve after 10 days.
Uncommon risks
- There is a very low risk of developing retrograde ejaculation this is much lower than the risk with TURP.
- In 1% of cases, patients can develop urinary incontinence.
- The prostate can become swollen immediately after the procedure, making passing urine difficult – a urinary catheter may be necessary until the swelling settles down.
- There is the possibility of having blood in the urine after PAE, this usually settles by itself.
- Blocking arterial flow to the prostate makes the gland more prone to infection – antibiotics will be prescribed for you to take after the procedure.
- There is a less than 1% risk of blocking blood vessels and blood supply to other organs inside your pelvis (including urinary bladder, bowels or genitals).
WHAT ARE THE RESULTS?
After PAE, the prostate gland should begin to shrink over the next few weeks. Studies show that more than 70% of men will see improvement in their symptoms after PAE.
Recent research has demonstrated that the majority of patients requiring a long term catheter can have this removed within a few weeks.
Difficulty in finding tortuous or small prostate arteries may lead to technical failures in around 10% of cases. In case of failure a traditional TURP surgery may be offered.



