Table of contents
DEFINITION
Uveitis is swelling and irritation (inflammation) in the eye. It often affects the middle layer of your eye (uvea) which is made up of three structures:
- The iris: the part of your eye that gives it colour;
- The ciliary body: a small ring-like muscle that sits behind your iris and which helps the eye to focus;
- The choroid: the layer of tissue between your retina and your sclera, containing blood vessels and a pigment that absorbs excess light.
The uvea contains most of the eye’s blood vessels.
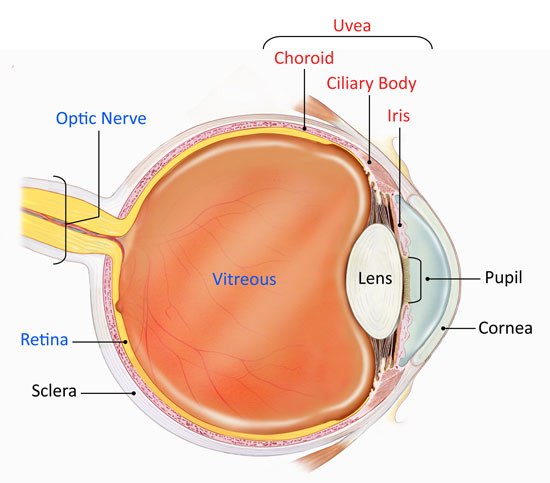
Uveal components
Uveitis can affect one eye or both eyes. It can cause short-term or long-term symptoms. Symptoms may go away and come back. Over time, the condition can damage or destroy eye structures and can lead to vision loss.
WHAT CAUSES UVEITIS?
This condition may be caused by:
- Infections that start in the eye or spread to the eye, and that may come from:
- A virus, such as shingles, mumps or herpes
- A fungus, such as histoplasmosis
- A parasite, such as toxoplasmosis
- A bacteria, such as syphilis, tuberculosis or Lyme disease.
- Inflammatory diseases which affect other parts of the body, such as arthritis, can also affect the eyes;
- Autoimmune diseases in which the body’s defense system (immune system) mistakenly attacks the body’s own tissues;
- Eye injuries:
- A result of injury to the eye
- Inflammation in one eye can result from a severe injury to the opposite eye (sympathetic uveitis).
However, in up to half of cases, no specific cause is found. This is known as idiopathic uveitis.
WHAT ARE THE SYMPTOMS OF UVEITIS?
Symptoms of uveitis include:
- Eye pain (usually felt as a dull ache in and around the eye);
- Redness of the eye;
- Blurry or cloudy vision;
- Light sensitivity (photophobia);
- Floating black spots across your field of vision (floaters).
The symptoms can develop suddenly or gradually over a few days.
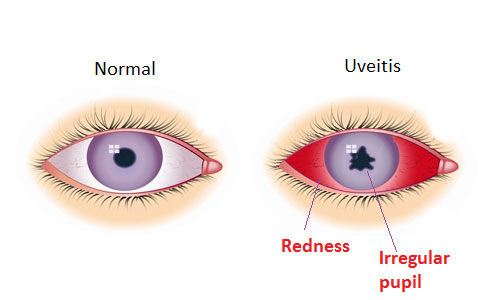
Symptoms
A case of simple “red eye” may in fact be a serious problem of uveitis. If your eye becomes red or painful, and does not clear up quickly, or if you have and unusual change in your vision you should be examined by an eye specialist (ophthalmologist). The sooner uveitis is treated the more successful treatment is likely to be.
HOW IS UVEITIS DIAGNOSED?
This condition is usually diagnosed by an ophthalmologist. The ophthalmologist will do a complete eye exam. This exam may include:
- A vision test using eye charts;
- An exam that involves using a scope for viewing inside the eye (ophthalmoscope or slit lamp). Eye drops may be used to widen (dilate) your pupil to make it easier to see inside your eye;
- A test to measure eye pressure.
You may need further investigations, especially if the ophthalmologist thinks there may be an underlying problem, if you have had previous episodes of uveitis, or if this episode is severe or affects both eyes. These tests may include Optical Coherence Tomography (OCT), which takes special pictures of your eye, blood tests and possibly also a chest X-ray.
You may have to see other medical specialists to determine an underlying condition.
HOW IS UVEITIS TREATED?
Treatment for uveitis aims to help relieve pain and discomfort in the eye(s), treat any underlying cause (if possible) and reduce the inflammation. This may prevent permanent loss of vision or other complications. Treatment usually includes the following:
Steroid eye drops
- Steroid eye drops are usually used to reduce the inflammation in uveitis. Steroid drops are the main treatment for uveitis and may be the only treatment for mild attacks. Examples of steroid drops include prednisolone and dexamethasone eye drops.
- Although steroid eye drops usually work well, in some cases side-effects occur and these are sometimes serious. Therefore, steroid eye drops are usually only prescribed by an eye specialist who can monitor the situation. It is particularly important to be certain that you don’t have herpes simplex virus (also called cold sore virus) infection of your eye before steroids are used.
- Possible side-effects that sometimes occur include ulcers on the cornea of the eye, which can be very painful and affect your vision. If steroid eye drops are used for long periods of time, they can lead to clouding of your lenses (cataracts) or to raised pressure in your eye (glaucoma).
Treatment to relieve pain and discomfort
- Cycloplegic eye drops: these are eye drops that relieve pain by causing the pupil in your eye to widen (dilate) by relaxing the muscle in the ciliary body. As a result, the inflamed iris is able to rest and recover. There are some side-effects. They can make your pupil appear large, and can cause temporary blurred vision and difficulty with focusing. When the effect of the drops wears off, these side-effects disappear. If these drops are not used, the inflammation in the iris may cause it to become ‘stuck’ to the lens, causing permanent scarring.
- Dark glasses: if your symptoms include sensitivity to bright light (photophobia), wearing dark glasses may be helpful.
- Painkillers: painkillers, such as paracetamol, may also help.
Steroids by mouth or injection
- In severe uveitis, steroids are sometimes given by injection into or around your eye.
- They can also be given by mouth. These can have side-effects when they are used for more than a few weeks. These include ‘thinning’ of the bones (osteoporosis), thinning of the skin, weight gain, muscle wasting and a generally increased risk of infection.
Immunosuppressive medicines
- If steroid treatment is needed in the longer term to treat uveitis, a second medicine known as an immunosuppressive medicine may be used.
- This can help to reduce the amount of steroids needed and/or help to control the uveitis if steroids are not working.
Treatment of underlying causes
- If there is an underlying cause of your uveitis this also needs to be treated (if possible).
- This means treating any underlying infection, inflammatory disease or autoimmune disease.
WHAT ARE THE COMPLICATIONS OF UVEITIS?
If uveitis is not treated quickly, it can lead to permanent loss of vision. It may also lead to complications, such as raised pressure in your eye (glaucoma). These complications can themselves affect your eyesight. If complications are not detected early, they can sometimes have a more harmful (detrimental) effect on your eyesight than the underlying uveitis.
The complications of uveitis may be caused by the effects of the inflammation inside the eye. Some of them may also be caused by the steroid treatment used to control the inflammation. Despite this, as a general rule, using enough steroids to control the uveitis will generally give a better outcome than using too few steroids and not controlling the inflammation. Complications that can sometimes occur with uveitis include:
- Formation of synechiae: the name ‘synechiae’ is given to the ‘bands’ of tissue that can form between the iris and the lens due to inflammation. Eye drops which cause the pupils to widen (dilate) help to prevent synechiae;
- Glaucoma: the inflammation in your eye may cause the pressure in your eye to increase and can cause glaucoma. Using steroids can also cause a sudden increase in pressure in your eye, especially if you already have glaucoma. If glaucoma is not treated, it can lead to loss of vision;
- Macular oedema: this is the term for fluid building up in the back of your eye around your macula on your retina. It may cause permanent visual loss. In addition, holes may form in the macula, leading to areas of lost vision on the retina;
- Cataract formation: eye inflammation can cause clouding of the lens (cataract formation). Cataracts may also be caused by long-term steroid treatment. If a cataract worsens and is not treated, it can lead to visual loss;
- Retinal detachment: the inflammation can cause ‘pulling’ on your retina so that it ‘comes away’ or is detached from the blood vessels below. This can cause you to experience flashing lights, floaters and problems with your vision. If you suspect that you have a retinal detachment, contact your ophthalmologist immediately, as urgent treatment is often needed.
WHAT IS THE OUTLOOK (PROGNOSIS) FOR UVEITIS?
In general, the sooner treatment for uveitis is started, the better the outlook and the quicker it goes away. However, uveitis can come back (recur), especially if it is associated with an underlying illness such as autoimmune or inflammatory disease.
Uveitis can sometimes become persistent (chronic) despite early and adequate treatment.
Some people who have recurrent uveitis learn to recognise their symptoms. They are sometimes given steroid eye drops to keep in reserve and start when their usual symptoms reappear. People who have chronic or recurrent uveitis are usually under the long-term care of an eye specialist and have regular check-ups in the outpatient clinic.
Uveitis caused by infection generally clears up when the infection is treated, and does not recur.



