WHAT IS AN ANAL FISSURE?
An anal fissure is a small tear in the thin mucosa that lines the opening of the anus (anal canal). Fissures typically cause pain and bleeding with bowel movements. Anal fissures are very common in young infants but can affect people of any age. Most anal fissures heal with simple treatments. Some people with anal fissures may need medication or, occasionally, surgery.
WHAT ARE THE SYMPTOMS OF AN ANAL FISSURE?
Signs and symptoms of an anal fissure include:
- Pain, sometimes severe, during bowel movements;
- Pain after bowel movements that can last up to several hours;
- Bright red blood on the stool or toilet paper after a bowel movement;
- Itching or irritation around the anus;
- A visible crack in the skin around the anus;
- A small lump or skin tag on the skin near the anal fissure.
WHAT CAUSES AN ANAL FISSURE?
Common causes of anal fissure include:
- Passing large or hard stools
- Constipation and straining during bowel movements
- Chronic diarrhoea
- Inflammation of the anorectal area, caused by Crohn’s disease or another inflammatory bowel disease
- Childbirth
- Direct trauma.
Other less common causes are anal cancer and certain infections (HIV, tuberculosis, herpes and syphilis).
HOW IS AN ANAL FISSURE DIAGNOSED?
If possible, your doctor will perform a digital rectal exam, which involves inserting a gloved finger into your anal canal, or use a short, lighted tube (anoscope) to inspect your anal canal. However, if this is too painful for you, your doctor may be able to diagnose an anal fissure only by observation.
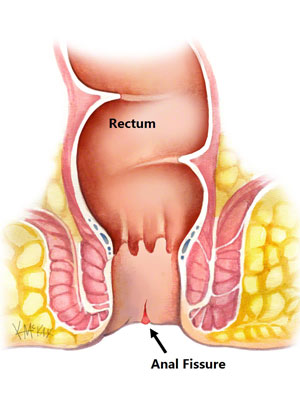
An acute anal fissure looks like a fresh tear, somewhat like a paper cut. A chronic anal fissure likely has the tear, as well as two separate lumps or tags of skin on both sides.
The fissure’s location offers clues about its cause. A fissure that occurs on the side of the anal opening, rather than the back or front, is more likely to be a sign of another disorder, such as Crohn’s disease. Your doctor may recommend further testing if he or she thinks you have an underlying condition, either flexible sigmoidoscopy or colonoscopy.
WHAT IS THE TREATMENT OF ANAL FISSURES?
Anal fissures often heal within a few weeks if you take steps to keep your stool soft, such as increasing your intake of fibre and fluids. Soaking in warm water for 10 to 20 minutes several times a day, especially after bowel movements, can help relax the sphincter and promote healing.
If your symptoms persist, you’ll likely need further treatment.
Nonsurgical treatments
- Fibre supplements: taking fibre supplements with fluids may help to keep soft stools and control constipation. Fibre obtained from food may cause much more bloating compared with a fibre supplement. Make sure you drink plenty of water when you take fibre supplement.
Example: Fructooligosaccharide (FOS) soluble fibre (NATUFIB) - Osmotic laxatives: if fibre doesn’t help symptoms, your doctor may prescribe an osmotic laxative which will pull water back into your colon, softens your stool so it is easier to get it out of your body and to make bowel movements less painful. Like fibre, just make sure you drink plenty of water when you take them to avoid getting dehydrated.
Example: Sorbitol, Lactulose - Topical anaesthetic creams may be helpful for pain relief.
Example: Lidocaine topical gel (XYLOCAINE JELLY) - Blood pressure medications can help relax the anal sphincter. These medications may be applied externally (not available in Vietnam) or taken by mouth.
Example: Nifedipine, Diltiazem, Nitroglycerin Jelly - Anorectal preparations: this type of medications is to relieve anal inflammation and rectal bleeding related to fissures.
Example: Diclofenac suppository (VOLTAREN) - Botulinum toxin type A (Botox) injection, to paralyse the anal sphincter muscle and relax spasms.

Surgery
If you have a chronic anal fissure that is resistant to other treatments, or if your symptoms are severe, your doctor may recommend surgery.
Doctors usually perform a procedure called lateral internal sphincterotomy which involves cutting a small portion of the anal sphincter muscle to reduce spasm and pain, and promote healing. Studies have found that for chronic fissure, surgery is much more effective than any medical treatment. However, surgery has a small risk of causing incontinence.



