During Delivery
Laparoscopic Morcellation
Wednesday, 11/08/2021 | Maternity | by FV Thomson
WHAT IS A LAPAROSCOPIC MORCELLATION?
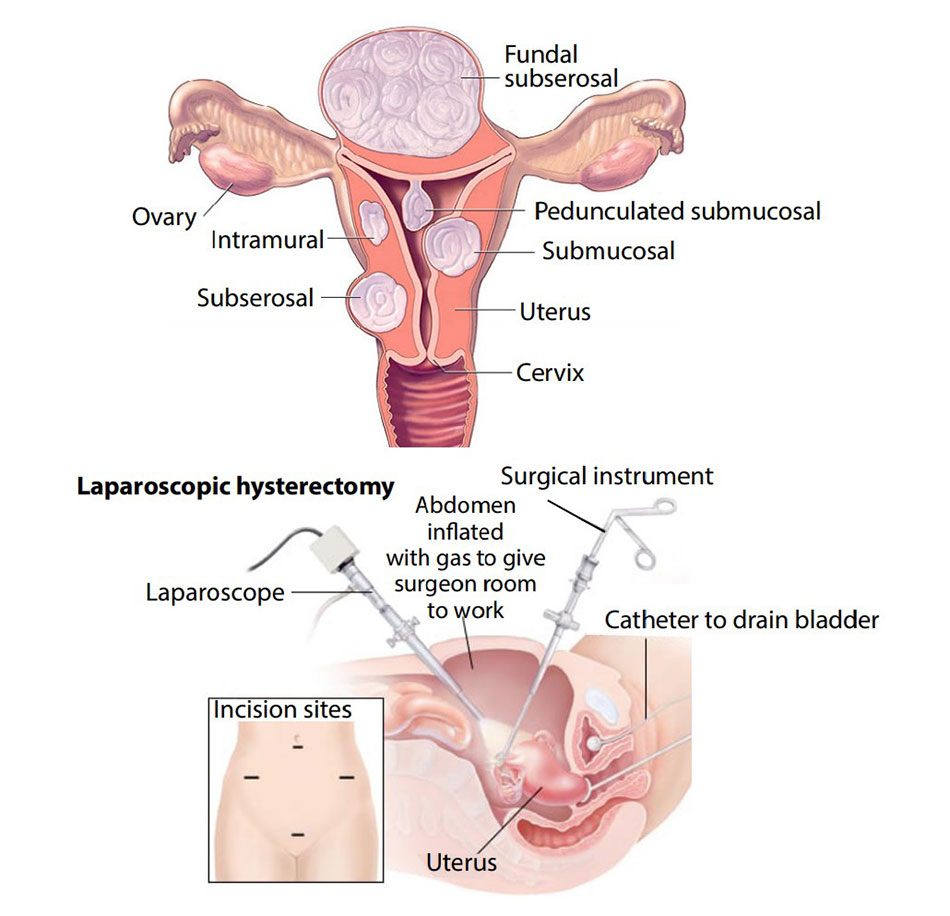
Laparoscopy is a minimally-invasive procedure in which small incisions are made in the abdominal wall through which a laparoscope – a thin tube with a light source and camera – and other instruments can be inserted. In this way, a number of surgical procedures can be performed without the need for a large surgical incision.
Morcellation is a tissue extraction technique to remove a large specimen through a small incision by cutting the tissue into small pieces by a ’morcellator’ with rapidly rotating blades.
WHAT ARE THE INDICATIONS OF LAPAROSCOPIC MORCELLATION?
Morcellation is usually only considered if you are having a laparoscopic total hysterectomy (surgical removal of your uterus) and your uterus is too big to be removed through your vagina, if you are having a laparoscopic subtotal hysterectomy (where the cervix is left in place) or if you are having a laparoscopic myomectomy (surgical removal of fibroids from your uterus).
WHAT ARE THE BENEFITS OF A LAPAROSCOPIC PROCEDURE?
Laparoscopic surgery has demonstrably better quality-of-life outcomes than open surgery and offers many advantages:
- Fewer risks and complications:
- The smaller incisions also reduce the likelihood of infection, because organs inside the body are not exposed to potentially contaminated air inside the operating room for a long period of time like it is in open surgery;
- Patients have fewer unwanted effects from analgesia because less analgesia is required;
- The incisions require less sutures to close them. This reduces the likelihood of complications from the wound, which are common in open surgery.
- Faster recovery: the length of hospital stay required is significantly shorter with laparoscopic surgery, since healing is so much faster;
- Less pain: the smaller wounds created in laparoscopic surgery means that patients almost always experience much less pain during the recovery period after their procedure. This means that they are less reliant on pain medications, and they will be able to get moving around much faster;
- Better cosmetic result: smaller incisions will leave a much smaller scar than those made in conventional surgeries.
WHAT ARE THE RISKS OF LAPAROSCOPIC MORCELLATION?
Laparoscopic morcellation in the right patients, with proper pre-operative investigations, carried out by experienced surgeons is a safe procedure.
Complications may include:
- Small pieces of benign (non-cancerous) fibroid or uterine tissue could be left inside your abdomen and may require additional surgery to remove them. The risk of this happening is thought to be between 0,1 and 0,8%.
- Morcellation of uterine tissue or fibroid that could contain an undiagnosed cancer called uterine sarcoma:
- Such an unsuspected cancer is very rare, the risk increases with age and is higher around the time of and after your menopause (estimated frequency is thought to be less than 0,5% before 50-years old, and about 1% after 60);
- Risk factors for uterine sarcoma are listed below;
- If an unexpected uterine sarcoma is morcellated, then it can potentially cause the cancer to spread and reduce the cure rate and survival.
WHAT MIGHT AFFECT MY RISK OF HAVING A UTERINE SARCOMA?
The following factors may mean that you have a higher risk of uterine sarcoma. Your doctor will check for these and discuss with you before considering morcellation:
- Fibroids that are growing quickly;
- Findings suspicious of uterine sarcoma on radiological investigations;
- If certain types of breast, ovarian or bowel cancer run in your family (such as BRCA mutations or Lynch syndrome);
- Your age, as your risk is higher around the time of and after your menopause;
- Your ethnicity-fibroids are more common in black women and the chance of uterine sarcoma may also be higher;
- If you have ever used the drug Tamoxifen;
- If your fibroid continues to grow despite medical treatment;
- If you have had radiotherapy to your pelvis;
- Bleeding after your menopause or irregular vaginal bleeding.
WHAT PRE-OPERATIVE INVESTIGATIONS MAY BE DONE BEFORE THE PROCEDURE?
Before considering morcellation, your doctor may offer you investigations that may include an ultrasound scan, a Magnetic Resonance Imaging (MRI) scan, an endometrial biopsy (biopsy of the uterus lining) and a cervical smear test. However, none of the currently available tests can reliably diagnose uterine sarcoma before surgery.
Overall, the risk from an undiagnosed cancer within a fibroid is extremely low, where patients have been fully checked and there is no suspicion of cancer, and must be considered in balance with the many advantages of laparoscopic morcellation.
WHAT ARE MY ALTERNATIVES TO MORCELLATION?
Your doctor will discuss with you the alternative options including having no treatment, ‘waiting and watching’, and open surgery where a larger cut is made on your abdomen to remove your fibroid or uterus in one piece.
WHAT ABOUT FUTURE PREGNANCY AND RISK OF UTERINE RUPTURE?
Laparoscopic myomectomy is a safe procedure from this point of view. Your surgeon will be able to advise you if an elective (planned) Caesarean Section is indicated or if you will be able to have a normal delivery.
WHAT ABOUT RECOVERY?
You will stay in the hospital for 48-72 hours depending on how well you recover. You may be in some discomfort especially on moving, but this will be well-controlled with analgesia. You may have light vaginal bleeding and some shoulder pain. You will feel tired, but will be able to eat and drink normally, walk around and go to the toilet. You will be discharged from the hospital after 48-72 hours.
For the first three days after discharge, we recommend taking regular pain-killers. You could take short walks, wash and shower as normal and avoid lifting heavy loads. You should also get plenty of rest (8 hours at night, 2 hours during the day). You will be seen at the end of first week for a post-operative review and suture removal.
You should gradually increase activity levels and should be able to return to work by four weeks.










