Vaginal birth: Labour and delivery
A vaginal delivery is childbirth that happens when the baby is pushed down the birth canal and delivered through the vagina. Every labour and delivery is different.
WHAT TO EXPECT TO PRIOR TO LABOUR
During pregnancy you should:
- Be sure to go to all prenatal care visits with your doctor
- Eat a healthful diet and drink plenty of fluids
- Get as much sleep as possible
- Read about giving birth and take a childbirth preparation class
- Choose a support person to be with you during labour and delivery
- Write a birth plan that explains what you want and helps you to think about possible complications
Talk to your doctor about:
- Ways to contact him/her after hours and when you should call
- Steps you should take when in labour
- Whether you want pain relief during labour
- Perineal massage, the perineum is the area between the anus and the vagina. Massaging it may help to reduce your chance of trauma to that area.
- How you will travel to the hospital
- Arrangements for home and work
- Be aware of the signs of labour, which include:
- Contractions
- Water breaks
- Back pain
- Slight vaginal bleeding
TRUE VERSUS FALSE LABOUR
Before true labour begins, you may have periods of false labour. These are irregular contractions of your uterus, called Braxton Hicks contractions:
- Usually they occur no more often than once or twice per hour, and often just a few times per day.
- They are irregular and do not increase in frequency with increasing intensity
- They resolve with ambulation or a change in activity.
- These contractions are normal but can be painful.
- They are usually also felt in the stomach and not the back.
Timing the contractions is a good way to tell the difference between true and false labour. Note how long it is from the start of one contraction to the start of the next. Keep a record for an hour. If the contractions are getting closer together, longer, stronger, and are being felt in your back, then it may be true labour. If you think you are in labour, call your doctor.
BIRTH LABOUR
How long labour and delivery lasts and how it progresses varies depending on previous births, the position of the baby’s head, and the size of the baby and the birth canal. The average time for you to deliver your first baby and the placenta is 12 hours. This can vary greatly, though. There are general stages of labour and delivery that a healthcare provider uses to decide whether it is progressing normally for a vaginal delivery.
The 3 stages of labour are:
- First stage: The cervix opens and thins to full dilation. The average woman in her first labour may dilate about 1 cm per hour during the active phase of labour. If you have had a baby before, the cervix usually dilates faster.
- Second stage: The baby moves through the birth canal and is born. This stage of labour usually lasts 15 to 75 minutes but may last as long as 2 or 3 hours.
- Third stage: The placenta (afterbirth) passes through the birth canal and is delivered. This usually happens within 30 minutes after the birth of the baby
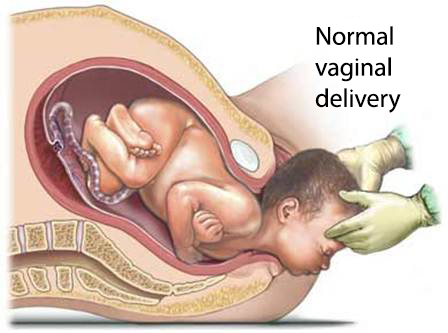
At the beginning of labour, the uterus (where the baby grows during pregnancy) will begin to contract, moving the baby down the vagina (birth canal). The cervix, the opening of the uterus into the vagina, will slowly enlarge to a diameter of about 10 centimetres. This will allow the baby to pass through and be delivered through the opening of the vagina. This process usually takes a while. However, if you have delivered vaginally before, labour can be quick.
When the cervix is fully dilated (opened) and the baby seems to be heading down the birth canal, the nurses will help prepare you for delivery. You will be positioned optimally, and your legs may be draped with cloths. Some doctors will clean the area around the vagina with an antiseptic solution.
You may put your legs into holders, especially if you have an epidural. The nurses and your support people may hold your legs in a comfortable position. This will help you to push. Your doctor may encourage you to find a position that is right for you. Each time you have a contraction, you will be instructed to push. This involves you bearing down, like you are trying to have a bowel movement.
“Crowning” is when the baby’s head is seen at the opening to the vagina. When this happens, you may be asked to slow your pushing. Depending on your delivery plan, the doctor may massage your perineum to gently stretch it. An episiotomy is not routinely done, but in some cases, it is necessary.
Once your baby’s head is out, you will be asked to stop pushing. The doctor will check to make sure that the umbilical cord is not around the baby’s neck. Then, you will be able to push the rest of the baby out. If the baby appears healthy and is breathing well, the baby may be placed on your stomach. The umbilical cord will be clamped and cut. Within the next 20 minutes, the placenta will be delivered.
Vaginal Birth
Sometimes the baby’s head does not move as expected through the birth canal. If this happens, your doctor may use forceps or vacuum extraction to deliver the baby.
ANAESTHESIA
Labour can cause severe pain, but keep in mind that every woman’s labour is different. Everyone experiences pain differently. While planning the delivery, talk to your doctor about your options for pain relief.
In the early stages of labour, techniques like rhythmic breathing, meditation, and acupressure may be helpful. Some women do not require any other pain control.
There are many medical options for pain control. All treatments to relieve pain during labour have risks and benefits. Make sure you discuss these with your doctor:
- Pain medications by IV or muscle injection:
- Given when contractions become stronger and more painful
- Can cross into the baby’s bloodstream
- Epidural block:
- Liquid pain medication injected near spinal cord
- Given in small amounts by an anaesthesiologist—a doctor who specializes in anaesthesia
- Does not cross into baby’s bloodstream
- Decreases pain and feeling in your lower body
- Provides good pain relief and allows you to continue with delivery
- Can cause headaches and drop in blood pressure, as well as changes in baby’s heartbeat
- Spinal block:
- Liquid pain medication injected into spinal fluid
- Used for pain relief during delivery, especially if forceps or vacuum extraction is needed
- Often used for C-section
- Numbs lower half of the body and reduces your ability to push
- Provides good pain relief and works quickly
- Can cause headaches after delivery and drop in blood pressure during labour and delivery, as well as changes in baby’s heartbeat
- Local anaesthesia:
- Injected into vagina or surrounding area
- Used if an episiotomy (cutting near the vagina) is needed
- Also used when vaginal tears are stitched
- Does not relieve pain of contractions during labour
POSSIBLE COMPLICATIONS
The second stage of labour may be delayed or lengthy due to:
- Malpresentation (breech birth (i.e. buttocks or feet first), face, brow, or other)
- Failure of descent of the foetal head through the pelvic brim or the interspinous diameter
- Poor uterine contraction strength
- Active phase arrest
- Cephalo-pelvic disproportion (CPD)
- Shoulder dystocia
Some factors that may increase the risk of complications include:
- Anaemia
- Diabetes
- Bleeding disorder
- Lung or heart disease
- Infectious disease, such as active genital herpes or HIV
- Water breaking before your contractions start
- Placenta positioned over the cervix — placenta praevia
- Early separation of the placenta from the uterine wall — placental abruption
- Umbilical cord slips out of the birth canal before the baby’s head — umbilical cord prolapse
- Large baby or a baby in the wrong position inside the womb
Immediately after birth
- Right after birth, your baby may be placed on your abdomen or chest. This skin-to-skin contact may lead to improved breastfeeding success.
- You may need stitches if your perineum is cut or torn.
- You may receive abdominal massage to help the uterus clamp down and decrease bleeding.
- The vaginal area, perineum, and rectum will be cleansed.
- An ice pack will be placed on the perineum to soothe and decrease swelling.
- You may be given a shot of oxytocin to help decrease bleeding.
- You will be given pain medication.
POST-BIRTH CARE
The usual length of stay for a vaginal delivery is 3-4 days. Your doctor may choose to keep you longer, however, if complications arise.
Postpartum is the time after the birth of your baby when your body is changing back to normal. It lasts about 6 weeks or until your uterus returns to its normal size. If you are not breast-feeding, you may start having menstrual periods 3 to 10 weeks after delivery. If you are breast-feeding, you may not get your period again until you stop breast-feeding. During this time, you will need to take steps to adjust to your body’s changes and life with a new baby.
Physical Effects
Physically, you might have the following:
- Sore breasts—your breasts may be painfully engorged when your milk comes in. Also, your nipples may be sore.
- Constipation —you may not be able to move your bowels until the third or fourth day after delivery.
- Stitches may make it painful to sit or walk.
- Haemorrhoids — Haemorrhoids are common. They may make it painful for you to move your bowels.
- Hot and cold flushes—this is due to your body trying to adjust to the change in hormones and blood flow levels.
- Urinary or faecal incontinence—during delivery, your muscles were stretched. This may make it hard for you to control your urine and bowel movements for a short period of time after delivery.
- After pains—the shrinking of your uterus can cause contractions. These can worsen when your baby nurses or when you take medication to reduce bleeding. It is normal to have this after delivery.
- Vaginal discharge—this is heavier than your period and often contains clots. The discharge gradually fades to white or yellow and stops within 2 months.
- Weight—your postpartum weight will probably be about 10 pounds below your full-term weight. Water weight drops off within the first week as your body regains its salt balance.
Emotional Effects
Emotionally, you may be feeling:
- “Baby blues”—about 80% of new moms have irritability, sadness, crying, or anxiety. This begins within days or weeks of giving birth. These feelings can result from hormonal changes, exhaustion, unexpected birth experiences, adjustments to changing roles, and a sense of lack of control over your new life.
- Postpartum depression (PPD)—this condition is more serious and happens in 10%-20% of new mothers. It may cause mood swings, anxiety, guilt, and persistent sadness. Your baby may be several months old before PPD develops. It is more common in women with a family history of depression.
- Postpartum psychosis—postpartum psychosis is a rare, but severe condition. Symptoms include difficulty thinking and thoughts of harming the baby. If you feel this way, call your doctor right away.
- Sexual relations—you may not feel physically or emotionally ready to begin sexual relations right away. In most cases, you will feel more interested in sex in a few weeks.
Ways to Take Care of Yourself
- When your baby sleeps, take a nap.
- Set aside time each day to relax with a book, or listen to music.
- Ask your doctor about when it is safe to shower, bathe, or soak in water.
- Get plenty of exercise and fresh air.
- Schedule regular time for you and your partner to be alone and talk.
- Make time each day to enjoy your baby. Encourage your partner to do so, too.
- Breastfeeding is encouraged unless your doctor tells you otherwise
- If you do breastfeed, ensure you clean the nipples before putting the baby to breast each time
- Take a break from having visitors if you feel stressed.
- Ask for help when you need it.
- Talk with other new moms and create your own support group.
- Delay having sexual intercourse and inserting any intra-uterine device for birth control until you have had your 4-6 week check-up
CALL YOUR DOCTOR
After you leave the hospital, contact your doctor or call the Obstetrics & Gynaecology Department if any of the following occur:
- Signs of infection, including fever and chills
- Increased bleeding: soaking more than one sanitary pad an hour
- Wounds that become red, swollen, or drain pus
- Vaginal discharge that smells foul
- New pain, swelling, or tenderness in your legs
- Pain that you cannot control with the medications you were given
- Pain, burning, urgency or frequency of urination, or persistent blood in the urine
- Cough, shortness of breath, or chest pain
- Depression, suicidal thoughts, or feelings of harming your baby
- Breasts that are hot, red, and accompanied by fever
- Any cracking or bleeding from the nipple or areola (the dark-coloured area of the breast)
If you think you have an emergency, call for medical help right away.
During Working Hours: + 84 8 54 11 35 35
Or call the 24/24h Hotline: +84 8 54 11 34 50