“Patient Kong Kham Pravong, a French national, was brought to FV Hospital’s Accident & Emergency Department in a critical condition marked by abdominal infection, severe malnutrition, and gastrointestinal bleeding, with a survival prognosis of only 20 per cent. FV’s doctors worked relentlessly for two months to save his life. Mr Kong underwent two surgeries, including the removal of his stomach, and received meticulous post-operative care.”
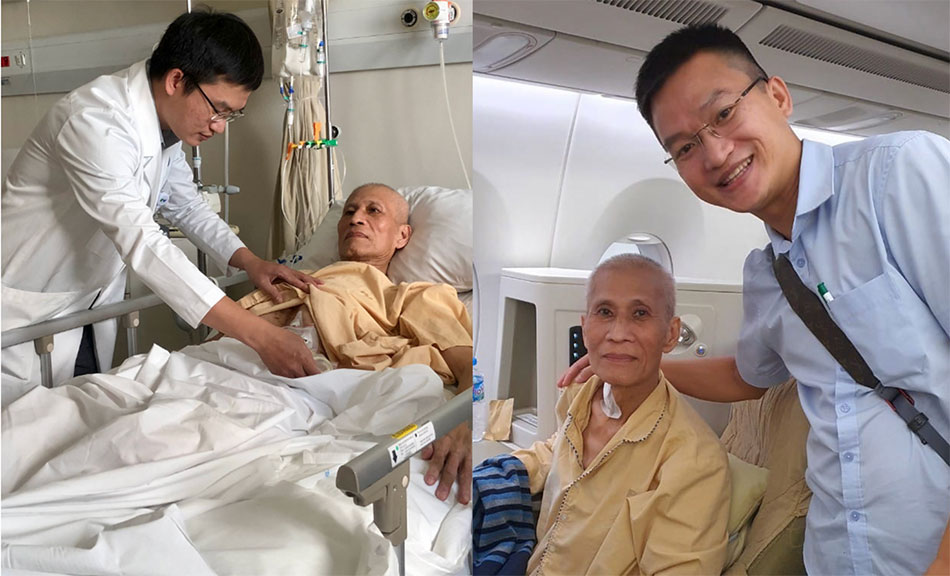
After saving Mr Kong’s life, FV doctors accompanied him on his flight back to France to ensure safety.
Two challenging surgeries to save a patient’s life
When Mr Kong Kham Pravong was admitted to FV Hospital on June 17th, Tran Xuan Tiem, a doctor at the General & Thoracic Surgery Department, described his condition as ‘the most severe I’ve ever seen.’
Before arriving, Mr Kong had undergone two surgeries in Cambodia to repair a perforated stomach, had his spleen removed, and had a feeding tube placed. However, complications arose. His family decided to seek treatment at a reputable hospital, and after much consideration, they chose FV Hospital.
Medical tests revealed that Mr Kong had an abdominal infection and a large hole in his stomach that measured seven centimetres in length, extending from the pylorus to the posterior wall of the stomach. He also presented with compression in the lower oesophagus-gastric junction and the pyloric canal, and leakage from the site of the feeding tube insertion. Additionally, Mr Kong was suffering from severe malnutrition and a severe fungal infection, and had significant muscle wastage. The medical team assessed his chances of survival at only 20 to 30 per cent.
A multidisciplinary team meeting was convened, attended by FV’s Medical Director and specialists from General & Thoracic Surgery, Anaesthesiology & ICU, Dietetics & Nutrition, and Infectious Disease departments. Based on clinical findings, the team unanimously agreed that rapid surgical intervention was the only chance to save the life of this 66-year-old man.
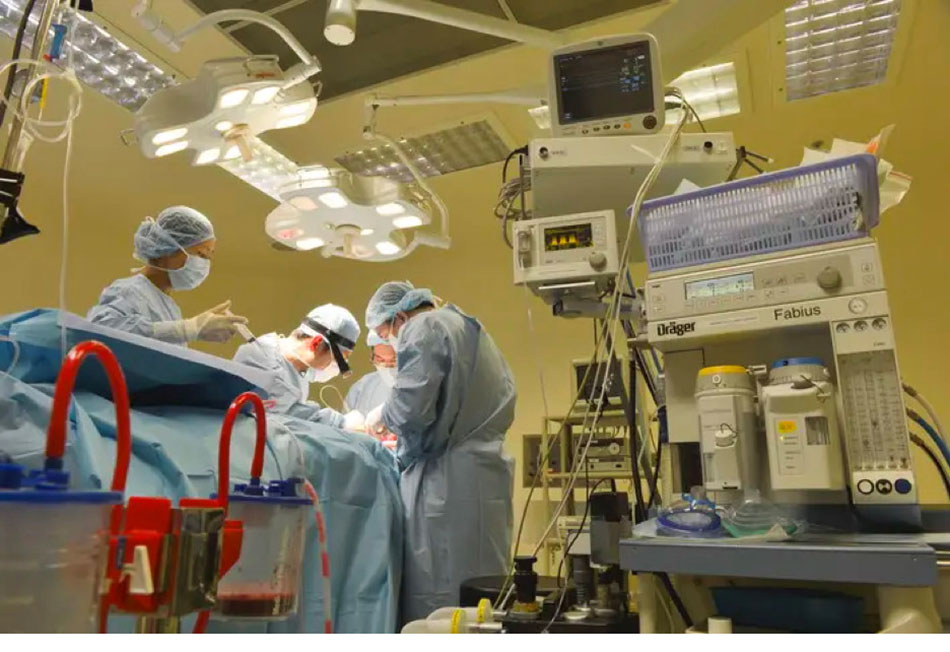 Doctors perform abdominal lavage as they remove the patient’s stomach during a six-hour surgery.
Doctors perform abdominal lavage as they remove the patient’s stomach during a six-hour surgery.
The six-hour surgery was conducted by Dr Le Duc Tuan and Dr Tran Xuan Tiem from FV’s General & Thoracic Surgery Department. When they opened the patient’s abdomen, they found a large perforation in the stomach which extended from the intersection of the cardia and posterior fundus through the body of the stomach. Initially, the surgical team suspected the hole might be due to cancer, in which case the patient’s chances of survival would have been extremely low. Fortunately, pathological examination revealed a benign lesion, and doctors were determined to do everything they could to save him.
“The patient’s abdomen was severely infected, and gastrointestinal fluids had spread throughout the abdominal cavity. Because the stomach was deformed, contracted and necrotic around the perforation site, we decided to completely remove the stomach, reposition the upper oesophageal stump, create a gastrostomy for feeding and a duodenostomy and jejunostomy, and establish abdominal drainage for the patient,” explains Dr Tiem.
Following surgery, Mr Kong received extensive postoperative care involving multiple specialties, including nutrition management, monitoring of the enteric system, infection control, and more, with the active involvement of both nurses and doctors.
However, one month later, the doctors discovered a leakage in the patient’s colonic flexure. Faecal material was leaking from a perforation in the colon into the upper abdomen, while the oesophageal stump and duodenal stump were also leaking into this area.
“This was dangerous because the area that we were diligently protecting from infection was being contaminated. Therefore, we were forced to perform a second surgery,” says Dr Phan Van Thai, Head of the General & Thoracic Surgery Department.

Dr Phan Van Thai and his team perform surgery.
In cases of colonic fistula in the abdominal cavity, surgical correction involves the widening of the incision to release the colon segment containing the perforation. However, due to the patient’s weakened condition after undergoing multiple surgeries, this conventional approach to access the site would likely compromise the protective abdominal wall that the medical team had worked diligently to maintain over the previous month. This could lead to the risk of a dangerous abdominal infection spreading, potentially resulting in a life-threatening situation.
Doctors decided on a less invasive, safer intervention: bringing the terminal ileum out through the skin (creating an artificial anus at the end of the small intestine) via a small incision. Simultaneously, they performed laparoscopic surgery localised to the infected colonic segment in the upper abdominal cavity. They thoroughly irrigated the area and established drainage systems to isolate and evacuate the infection site, preventing any further leakage into the abdominal cavity and the associated risk of a dangerous infection. Mr Kong remained stable during the four-hour surgery and his post-operative recovery went well, his condition gradually improving, day by day. Doctors tailored this care protocol uniquely to suit this unique situation, as there were no established guidelines in the medical literature.
“We had to choose the most appropriate approach for this special case based on our knowledge and experience,” recalls Dr Thai.
These surgeries were extremely challenging, but post-operative care was even more intricate, as doctors and nurses paid meticulous attention to every detail to save the patient’s life.
While surgery is considered the major factor in saving the patient’s life, Dr Tiem says that Mr Pravong’s successful recovery after surgery was greatly dependent on post-operative care, which was conducted with utmost diligence and caution. Each day, two nurses and one caregiver changed the bandages three times, performed irrigations, and drained fluids through the catheters. They also rotated Mr Kong to prevent bedsores and ensured that he received the correct doses of antibiotics and antifungal medications.

Dr Tiem conducts a final examination before Mr Kong is discharged.
In addition, nutrition plays a crucial role in recovery. Mr Kong was fed intravenously and through a feeding tube, with the dosage carefully calculated by the Dietetics & Nutrition Department.
Reflecting on taking care of Mr Kong for the previous two months, nurse Pham Thi Thanh stated, “In 20 years of my career, I’ve never seen a patient with so many tubes.” The team’s task was to ensure regular tube flushing, prevent infections, provide proper nutrition, and administer medication on time, without any room for error.
“Cases like this are very prone to infection, so the team must be attentive and carefully observe every little detail: from stool colour, urine colour, skin colour, to the placement of the tubes and IVs,” shares Ms Thanh.
If a tube or thread became twisted, it could cause pain for the patient. Inexperienced individuals might administer pain relief medication unnecessarily, but the solution is simply to adjust the direction of the tube or thread.
“This care is extremely complex. Each flushing session requires 1,000 to 3,000 millilitres of water and takes up to two hours to complete, and must be conducted two or three times a day,” explains Ms Thanh.
Mr Kong regained the ability to sit and move within a small range, engaging in physical therapy to restore function. Observing the patient’s transformation from a life-threatening condition, extreme weakness, and complete dependence on doctors and nurses, to being able to move again, was a source of indescribable joy for Ms Thanh. She takes pride in working with a highly skilled and dedicated team to care for patients and finds happiness in witnessing the remarkable recovery of those who were once predicted to have only “a few days to live.”
FV doctors accompany Mr Kong to France to ensure his safety during the journey
Mr Kong Kham Pravong’s treatment is not yet complete. FV doctors estimate that in about a year, when his physical condition has improved, he will need to undergo another surgery to re-establish his digestive tract, reconnecting the oesophagus to the small intestine. At that point, he will be able to eat through his mouth and have regular bowel movements through the anus.
Due to financial difficulties, the patient has only paid 20 per cent of his hospital fees. The family wishes to bring him back to France for follow-up and the surgery to restore the digestive tract, while also completing the necessary procedures with the French social insurance system to reimburse the remainder of the fees to FV.

Dr Tiem accompanies the patient to France on August 23, 2023.
“While the patient faced financial difficulties, the hospital’s principle is to always prioritise the patient’s well-being and life above all else, so the hospital focused on treating the patient first and settling fees later,” says Dr Phan Van Thai, Head of the General & Thoracic Surgery Department at FV Hospital.
“I am much healthier now compared to two months ago, and I no longer experience pain. I am aware of the severity of my illness. Seeing the doctors’ efforts motivates me to try my best to get better. The nursing staff is dedicated, available day and night, whenever needed. The quality of service at FV Hospital is on par with hospitals in France, and the standard of patient care is excellent. I am very grateful and want to express my thanks to the doctors, nurses, and aides at FV Hospital,” says Mr Kong Kham Pravong emotionally before his discharge.
On the flight to France on the evening of August 23, Dr Tran Xuan Tiem accompanied him, ensuring his well-being until he safely reached the airport in France. Subsequently, Mr Kong Kham Pravong was received by a large hospital in Paris. FV Hospital also coordinated the transfer of his medical records to the doctors in France for the convenience of planning his further treatment.



