Diagnosed with stage B liver cancer and inoperable, an 89-year-old man was treated with Transarterial Chemoembolization (TACE) at FV Hospital. After the first procedure, the tumour size had shrunk by over 90%.
During a routine health check, patient was shocked to discover a 3 cm liver tumour.
Mr T.N.T, 89 years old, decided to undergo a health screening at FV Hospital while accompanying his wife to the hospital for her medical check-up. The results revealed a malignant liver tumour about 3 cm in size.
Mr T’s case was discussed during FV Hospital’s regular multidisciplinary Tumour Board meeting, which is a weekly consultation where oncology, internal medicine, surgery, diagnostic imaging, and vascular intervention specialists collaborate to determine the best treatment approach for cancer patients.
After thoroughly evaluating Mr T’s condition, the Tumour Board concluded that his tumour was not suitable for surgery. They recommended treating his liver tumour using Transarterial Chemoembolization (TACE), a minimally invasive technique specifically for hepatocellular carcinoma cases that are not suitable for surgery.
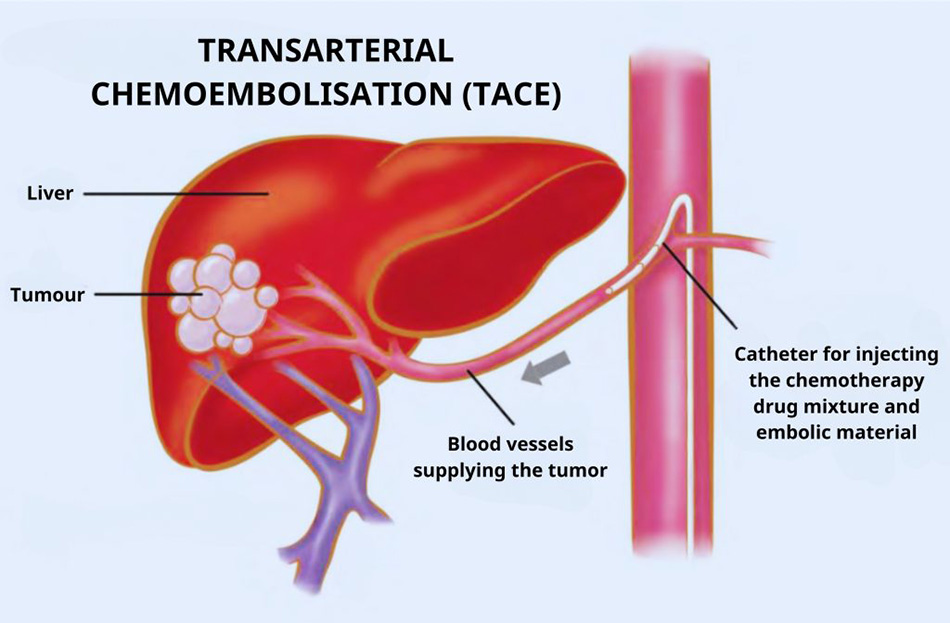
Illustration of the Transarterial Chemoembolization (TACE) liver procedure.
Dr Huynh Huu Danh – Diagnostic and Interventional Radiologist, Imaging and Interventional Radiology Department and the lead doctor in the team performing the TACE procedure on Mr T, told us: “The process of performing the TACE liver embolisation for Mr T was reasonably complex due to his kidney failure. We had to carefully adjust the contrast agents and chemotherapy medication to administer just the right amount, ensuring the procedure could be completed effectively while preventing further deterioration of his kidney condition.”
More than 90% of the tumour had disappeared one month after undergoing the TACE procedure.
The TACE procedure was performed by FV Hospital’s interventional radiology team. Through a small injection site in the patient’s right femoral artery, the interventional radiologist guided a catheter into the patient’s arterial system. Using contrast dye, the doctor created a detailed vascular map of the patient with the help of the DSA machine. With this vascular map, the catheter and micro-catheter were directed to the branch of the artery supplying blood to the liver tumour, where a mixture of chemotherapy drugs and embolic agents was injected to block the tumour’s blood supply.
TACE is a minimally invasive, non-surgical procedure that requires only local anaesthesia, allowing for a quick recovery after the intervention. Since it’s minimally invasive, patients experience no pain during the procedure.

Dr Danh and the DSA team are performing the procedure for the patient.
The patient’s health is stable after the procedure. “After the embolisation, Mr T’s recovery was quick, with no complications, especially no progression to acute kidney failure, which was a significant success for the entire team,” Dr Danh said.
“To achieve a successful procedure, it was due to the seamless and professional collaboration of the entire team at FV Hospital, including oncologists, general surgeons, gastroenterologists, radiologists, and the Cathlab team. I truly feel fortunate to work with such a professional team,” Dr Danh added.
One month after the procedure, Mr T underwent an MRI check-up. The MRI results were evaluated by the radiologists, who confirmed that the tumour had been reduced by over 90%.
Dr Danh assessed, “The patient will need to undergo at least one more TACE procedure to completely control the tumour and prevent recurrence.”
Upon receiving the follow-up results, Mr T and his family members were delighted that his condition had improved beyond expectations. Mr T expressed appreciatively, “I find the quality of FV Hospital very good, from the medical staff to the nurses and technicians; they are very dedicated and skilled. I place my trust in the doctors at FV, especially Dr Danh, a very talented young doctor.”

The patient had a follow-up appointment with Dr Danh one month after the first TACE procedure for liver embolization.
This is one of many cases that affirm FV ability to offer various personalised treatment options for each patient, particularly for cancer-related conditions.
Statistics show that liver cancer is the most prevalent type of cancer in Vietnam, with 90% of liver cancer cases being hepatocellular carcinoma (HCC). According to Globocan (the International Agency for Research on Cancer), According to the 2022 statistics from the Global Cancer Observatory (GLOBOCAN), Vietnam recorded 180,480 new cancer cases, with 120,184 fatalities, accounting for 66.7% of the cases.
“Liver cancer often presents with no clear symptoms and is usually detected when patients undergo screening. In Asia, liver cancer typically arises in individuals with cirrhosis or chronic hepatitis B and C infections. As such, this group should undergo regular annual screenings to detect the disease at an early stage. If the disease is not detected early, the tumour may grow and cause pain in the liver area or the right upper quadrant, making treatment more complex,” advised Dr Pham Dinh Khuong – Imaging and Interventional Radiology Department.
For more information about the TACE embolisation procedure for treating liver cancer, please contact Imaging and Interventional Radiology Department, FV Hospital at: (028) 35 11 33 33 – Ext. 1201 or 2222.



